Case of the month : Syncope on exertion :can he go Home?
| Contributed by DR PAREY MOHD FAROOQ
Clinical scenario : A 78 year old male brought into the emergency department by ambulance .Paramedics report that bypassers called EMS after witnessing a man collapsing in a park . As per eye witnesses he had brief shaky & jerky movements in upper and lower limbs .Couldn’t speak, was a bit confused for a while. & recovered gradually When EMS (Emergency medical services) arrived he was conscious & alert ,feeling slightly lightheaded .. He was otherwise hemodynamically stable. BP=101/67 ,Heart rate=56 regular, Spo2=97 , Temp=36.6 ,Random blood sugar =6.2 , GCS=15 /15 The patient reported that while walking briskly in the park he felt heart racing and then if it stopped beating .He was clammy ,diaphoretic ,and severely dizzy.The next moment found himself on the ground .He couldn’t recall events but thinks that he had a brief fainting attack.. He said he tried to speak but couldn’t and was unable to get up .He could recall that bypassers dragged him to nearby chair. He felt that his arms & legs were extremely weak. He recovered and gradually returned to his baseline within a few minutes. He denied having any chest pain,shortness of breath prior to collapse ,.He didn’t experience any Headache or Neck pain either. He felt nauseous prior to collapse otherwise denied any vomiting or abdominal pain,No Tongue bite ,bladder or bowel incontinence Past medical history Hypertension ,Dyslipidemia ,Osteoarthritis both knees Ex smoker ,drinks occasionally, denies drug abuse .Lives with his wife in a bungalow ,no mobility issues Medications ; Amlodepin,Rosuvastatin ; No allergies Clinical course : On arrival at the Emergency Department he was quite comfortable,clinically asymptomatic and hemodynamically stable . On detailed Physical exam , Conscious, alert and oriented ,His pupils were equal & reactive and he had no motor or sensory deficit He had no Primary or gaze evoked nystagmus and cerebellar signs were normal His respiratory and cardiovascular examination was unremarkable .His abdomen was soft and lax , There was no lower limb edema/swelling
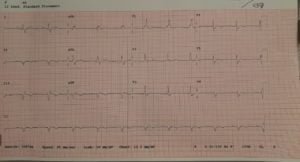
• His Blood gas showed Ph=7.38., Hco3= 24. With normal Pco2 and Lactate .His Fbc showed wbc= 7,5 Platelets=188 . Hgb= 156. .His renal function was unremarkable , His electrolyte panel was reported within normal limits ( Na= 138 K=4.5 Chloride=102.). • He had normal Liver function tests and coagulation profile. His Troponin was negative and D-dimer levels were normal . • The ECG was seen & signed by Physician and • signed as Sinus Rhythm /Right bundle branch block
NCCT brain was obtained ,while awaiting reports, the patient was handed over to night shift to chase the CT report with the clinical impression of Reflex syncope most likely Vaso-vagal . CT brain reported normal by radiologist on duty . When the discharge notes were updated in the system the nurse reported that patient while going to bathroom patient felt severely dizzy, diaphoretic ,cold and clammy Alarm button was pushed by staff and patient was rushed to resus room By the time his symptoms had improved, however was complaining of Palpitations His heart rate was about 138 with normal blood pressure and oxygen saturations .He was attached to cardiac monitor and an ecg was obtained immediately .The ECG was interpreted by Senior Physician as Bifascicular block (Sinus Tachycardia, Left axis deviation RBBB, LAFB )
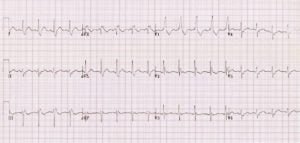
The Clinical impression and recommendation of hospital admission were noted in clinical charts & patient was referred to internal medicine . It was Specifically mentioned in notes due to high risk of progression to complete AV block the patient requires admission for possible Permanent pacemaker insertion/ EPS studies and cardiology review A week later patient collapsed while on evening walk .He was brought to ED, Hypotension & bradycardia ,.The ECG findings were consistent with Bifascicular block and third degree AV block . Due to adverse features of hypotension and decreased perfusion four doses of Atropine 0.6 mg were administered as per Uk resus guidelines however there can no significant improvement , The pacer pads were placed and pacing initiated , The patient was stabilized in emergency department and shifted to CCU .He underwent PPm Insertion without any complications was discharged in a good condition
Discussion : Bifascicular block is the combination of RBBB with either LAFB or LPFB When these occur in combination, significant conduction disease is usually present, and there is a risk for higher degrees of atrioventricular block in the future The term “Trifascicular block” is incorrectly used to define Right Bundle branch Block, Left Anterior Fascicular Block, and First Degree AV Block. The term in this context is a misnomer. First degree AV block is not a true block because there ere is a 1:1 relationship between P-waves and QRS The American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society (AHA/ACCF/HRS) recommends against the use of the term “trifascicular block”, as it does not have a unique anatomical association and does not accurately reflect the underlying anatomical disease process Learning points” 1)Bifascicular block with first degree AV block is inappropriately called “Trifascicular block,” a known misnomer. 2) Bifascicular block in context with syncope can be due to reversible causes like Myocardial ischemia, medications , and Hyperkalemia 3) If a patient with Bifascicular block ” develops complete heart block, it is likely to be infra-hisian and therefore atropine will not work, and pacer pads must be placed accordingly 4)Patients with bifascicular block and syncope or presyncope should be admitted for monitoring and likely pacemaker insertion (class II) 5) Asymptomatic bifascicular block with first degree AV block is not an indication for pacing (class III)
View in browser :The Health Guide |
Join the mailing list!
Get the latest articles delivered right to your inbox!