
Case of the month :Unmasking the Challenges of Posterior Circulation Stroke: A Case report
CONTRIBUTED By
Dr Mohd Farooq Parey ,MD MRCEM,FRCEM ,
Specialist Emergency medicine in University Hospital of Morecambe bay
NHS foundation Trust ,UK
Dr Malik Aftab ,MBBS,MRCEM ,
Specialty Doctor Emergency medicine University Hospital of Morecambe bay
NHS foundation trust
Abstract:
This article delves into a compelling case of posterior circulation stroke of vertebrobasilar territory encountered in the emergency department, shedding light on the intricate details of its presentation, diagnostic journey, and the unfortunate outcome. Through this case, we aim to highlight the importance of recognizing atypical symptoms associated with posterior circulation strokes, emphasizing the need for timely intervention
Introduction:
Posterior circulation strokes pose a unique set of challenges, often presenting with non-specific symptoms that can be misleading. This is a case of vertebrobasilar stroke, involving a patient with a history of previous PCA infarction, who ceased antiplatelet therapy in preparation for a procedure, only to manifest with acute neurological symptoms.
Case Presentation:
A 65-year-old man, previously diagnosed with hypertension and a history of a CVA in 2012 (PCA infarction), presented to the emergency department after experiencing dizziness and vomiting during his routine evening walk. Despite being on Clopidogrel, he had stopped the medication a week prior due to an upcoming prostate biopsy. Upon arrival at the emergency department, he was conscious, alert, and hemodynamically stable, with a blood pressure of 170/87, heart rate of 78, and normal temperature. His systemic examination revealed no remarkable findings, and neurological assessments, including NIHSS and NEWS, scored at 0.
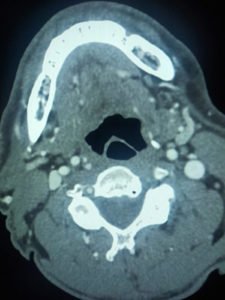
CT head was performed on arrival, showing no acute issues.
However, clinical suspicion of a posterior circulation stroke led to the activation of the Tele Stroke pathway.
The patient fell within the thrombolysis window, and after consultation, a Tele Stroke expert agreed to initiate IV thrombolysis.
The patient was moved to the resuscitation room for thrombolysis, where 6.9 ml of Alteplase bolus was administered, followed by a 62.4 mg infusion.
The plan was to admit the patient, but complications arose as he developed a headache and became sleepy and drowsy during the ongoing infusion.
The infusion was promptly halted, and a CT head was ordered to investigate the possibility of hemorrhagic transformation, which yielded negative results.
Despite these efforts, a subsequent CT angiogram revealed extensive basilar and vertebral thrombosis, leading to consideration for thrombectomy.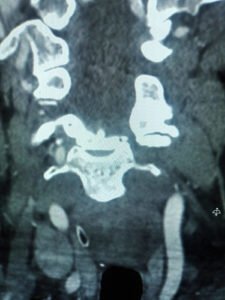
Unfortunately, the patient’s condition worsened, and thrombectomy wasn’t feasible due to the territory of the infarcts. The patient was made comfortable and passed away shortly thereafter.
Conclusion:
This case serves as a poignant reminder of the complexities associated with posterior circulation strokes. The higher mortality rate, as evidenced in this instance, accentuates the need for increased awareness, early recognition, and tailored intervention strategies. By sharing and reflecting on such cases, we strive to enhance our understanding and ultimately contribute to improved patient outcomes. Stay informed, stay vigilant.
References
Edlow, J. Managing Patients With Acute Episodic Dizziness. Ann Emerg Med. 2018;72;602-610. Newman-Toker, D.E., Hsieh, Y.H., Camargo, C.A. Jr. et al. Spectrum of dizziness visits to US emergency departments: cross-sectional analysis from a nationally representative sample. Mayo
Join the mailing list!
Get the latest articles delivered right to your inbox!


