
Undifferentiated Hypotension: How an Ultrasound clinched the diagnosis.
Contributed by
Dr Parey Mohd Farooq MD,MRCEM
Associate specialist Emergency medicine
Educational and training lead Emergency Department
Royal Lancaster Infirmary
University Hospital of morecambe bay NHS foundation trust -United kingdom
Clinical scenario : A 62 year old male was referred by his GP for evaluation of fainting episodes .He arrived at the Emergency department with his neighbor .While in the waiting room ,getting to be triaged he was witnessed to have a brief fainting episode by his friend and immediately brought in to Resus .He felt short of breath and his heart was racing ,and he was light headed .He couldn’t fully recall the events but thought he had a brief fainting episode .
Collateral hx from his friend who noticed him stumbling towards his right side with brief shaky jerky movements mainly on right side for less than a minute .His eyes were unrolling and he didn’t have any frothing .He recovered immediately within a minute without any post ictal confusion
In the Resus he was feeling well but complained of lightheadedness and mild shortness of breath .He was noticed to be hypotensive with blood pressure of 97/64 ,His heart rate was 144 , and Spo2=94% on room air , He was afebrile and his temp was 36.6
He was attached to a cardiac monitor ,IV access was obtained , blood samples were obtained accordingly .A bolus of Isotonic fluid was initiated and 12 lead ECG was recorded (figure 1).
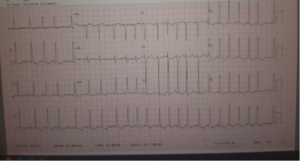
ECG interpretation :
Normal axis ,irregularly irregular rhythm heart rate 138 , widespread t wave inversion s, normal qrs
ECG diagnosis : Atrial fibrillation with Rapid ventricular response
Past medical hx & clinical course
Long standing Diabetes on metformin and insulin .He is also known to have Hypertension on Ramipril .
Non smoker ,denied any illicit drug use and drank occasionally at social events .
Two days prior to current presentation he collapsed in his bedroom when his wife was in kitchen .
He couldn’t recall the events but his wife thought he had a brief seizure .No tongue bite or incontinence reported .Since then he had been having intermittent palpitations and shortness of breath .
Clinical course : While in the Resus room his blood pressure started to pick up with IV fluid bolus ,however his heart rate continued to be rapid and irregular .
His blood results revealed leukocytosis with normal neutrophils .
His CRP was 206 (grossly elevated ) .Renal & liver function was normal .His X-ray chest was reported unremarkable .His urine dipstick was negative for
leucocytes ,nitrites and blood .
At this point of time two differential diagnosis were presumed
1.Sepsis precipitating Atrial fibrillation.
2.AF with rapid ventricular response with adverse features( hypotension )
Antibiotics were commenced although there was no focus of infection as such .it was decided that its sepsis precipitating AF so rate or rhythm control was not required .There were no other adverse features which would have indicated synchronized cardioversion.
After discussing the patient with the senior registrar of internal medicine it was decided to admit the patient as Sepsis .
While the patient had been waiting for bed in the Acute medical unit the nurse incharge reported that the blood pressure of the patient had dropped further to 87/46 .
Despite the repeated bolus and ongoing isotonic fluids, the patient continued to drop his blood pressure while his SPo2 continued to be 93% and his heart rate remained irregular at 144 .Due to drop in blood pressure reassessment Senior emergency physician Opinion was sought
Rapid ultrasound for shock and hypotension (RUSH protocol) was performed accordingly .
The findings revealed normal LVEF , however RV was found to be dilated with RV size more than LV ,flattening of interventricular septum was noticed .
There was no pericardial effusion, IVC was normal .There was no free fluid .Lung sliding was present and there were no radiological signs of pneumothorax , Abdominal aorta was less than 2.5 cm .
Considering the positive findings of RV strain in RUSH protocol , a CT pulmonary angiogram was requested .
It was reported as bilateral pulmonary embolism causing RV strain , The patient was immediately started on a treatment dose of enoxaparin . His blood pressure improved gradually and he was admitted to AMU in stable condition ;
Learning points :
1.POCUS is ideal for quick evaluation of haemodynamic status in the patients in emergency settings with undifferentiated shock
2.RUSH protocol is a prompt diagnostic tool and a broad ultrasound which addresses patients with hypotension and shock
3.Whenever hypotension worsens after iv fluids ,think about PE as volume resuscitation over distends the RV and reduces filling of Left ventricle leading to reduced cardiac output
- AF usually develops secondary to PE due to right atrial distention however its may cause PE as well
- The relationship between PE & AF is poorly studied and may require further research
References ;
- https://onlinelibrary.wiley.com/doi/pdf/10.1111/ j.1538-7836.2011.04608.x
- https://pubmed.ncbi.nlm.nih.gov/28196379/
- https://www.ahajournals.org/doi/10.1161/ JAHA.117.006502
- https://emcrit.org/rush-exam/
- https://www.aliem.com/rush-protocol-rapid- ultrasound-shock-hypotension/
View in browser :The Health Guide
Join the mailing List of The Health Guide
Join the mailing list!
Get the latest articles delivered right to your inbox!



