
Previously misdiagnosed as Chronic liver disease.
Clinical scenario :
A 19-year-old male was referred to our hospital with a one-year history of breathlessness on exertion and fatigue, accompanied by a history of gastrointestinal bleeding. Three months ago, he experienced three episodes of painless hematemesis, during which he was admitted to another hospital and diagnosed with variceal bleeding. At that time, he received four units of blood transfusion and underwent two sessions of variceal band ligation.
Subsequently, he developed progressive abdominal distension and pedal edema about a month later, for which he was started on diuretics. He denied symptoms of jaundice or altered sensorium. Notably, there was no history of diarrhoea during childhood, and his physical growth reported as normal. At the referring hospital, he was diagnosed with chronic liver disease.
Examination
On examination at our hospital, the patient presented with pallor and mild icterus but no pedal edema. His blood pressure was 120/80 mm Hg. Abdominal examination revealed hepatomegaly (3 cm below the right costal margin), splenomegaly (4 cm), and shifting dullness indicative of ascites.
Laboratory investigations showed severe anemia with a hemoglobin level of 6 g/dl, a total leukocyte count of 3200/mm³, and a platelet count of 1.75 × 10⁵/mm³. Peripheral blood smear demonstrated hypochromic microcytic red blood cells.
Liver function tests revealed a serum bilirubin level of 5.4 mg/dl, aspartate aminotransferase (AST) of 81 IU/ml, alanine aminotransferase (ALT) of 136 IU/ml, alkaline phosphatase of 164 KAU/dl (reference range <30 KAU), and hypoalbuminemia with a serum albumin level of 2.5 g/dl and globulins of 3.5 g/dl.
Ascitic fluid analysis showed a wide serum-ascites albumin gradient (SAAG), and there was no evidence of spontaneous bacterial peritonitis (SBP).
Viral hepatitis screening for hepatitis B surface antigen and anti-hepatitis C virus antibodies was negative. Serum ceruloplasmin levels were normal (34 mg/dl), and slit-lamp examination revealed no Kayser–Fleischer ring. Autoimmune markers were also negative.
Imaging studies included an ultrasound of the abdomen, which showed hepatomegaly (13.6 cm) with a coarse echo texture. All three hepatic veins appeared attenuated with comma-shaped collaterals, and intrahepatic biliary radicals were not dilated. Splenomegaly was noted, with a splenic vein diameter of 14 mm. Moderate ascites and multiple spleno-renal collaterals were present.
MRI of the liver corroborated the findings, revealing non-visualization of the hepatic veins and the presence of patent inferior vena cava, consistent with Budd-Chiari Syndrome. MR venography confirmed the absence of hepatic vein visualization with a patent inferior vena cava (Fig. 1a and b).
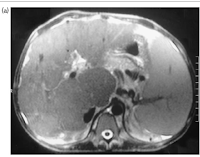 |
| Fig 1 MRI showing non visualisation of hepatic veins |
 |
| Fig 1 B MR venography showing non visualisation of hepatic veins |
Investigations for a hypercoagulable state demonstrated functional deficiencies of protein C and protein S, but the patient tested negative for lupus anticoagulant and the factor V Leiden mutation.
An upper gastrointestinal endoscopy revealed three streaks of small esophageal varices and evidence of mild portal hypertensive gastropathy. Notably, grooving and scalloping were also observed. These findings further underscore the presence of portal hypertension and its complications.
 |
| Fig 2 Endoscopy showing features of Celiac disease |
In the second part of the duodenum (Fig. 2), grooving and scalloping raised a suspicion of celiac disease. Biopsies were taken, and histological examination of the duodenal samples revealed hallmark findings of celiac disease, including increased intraepithelial lymphocytes, crypt hyperplasia, and subtotal villous atrophy.
Serological tests supported the diagnosis, with markedly elevated serum IgA anti-tissue transglutaminase antibody titers (>300 units/ml, cutoff 50 units/ml) and positive IgA anti-endomysial antibodies.
Treatment was initiated with oral anticoagulants, alongside a gluten-free diet and nutritional supplementation.
Ten months later, the patient showed significant clinical improvement. He reported feeling better overall, had gained weight, and had no signs of ascites.
His hemoglobin level increased to 12 g/dl, and his total leukocyte and platelet counts normalized. Liver function tests also showed improvement, with a serum albumin level rising to 3.4 g/dl. The patient’s recovery brought a visible sense of well-being, marked by a broad smile of satisfaction.
Message : This 19 year old boy had not chronic liver disease , instead he had celiac disease giving rise to Budd Chiari syndrome .He responded to gluten free diet and vitamin supplementation
“Don t go by the label ensure proper diagnosis in every case”
View in browser :The Health Guide
Join the mailing List of The Health Guide
Join the mailing list!
Get the latest articles delivered right to your inbox!


