Case of the Month : Sudden onset swelling in a Young man , a rare syndrome revisited
Contributed by
Dr Ali Al Ahmari Head of the dept of Gastroenterology AlHADA Military Hospital Saudi Arabia
CLINICAL SCENARIO
A 37-year-old male, presented with sudden onset swelling of arm and presence of prominent veins on the left arm as shown in .Fig.1
He denied history of trauma and had no co morbid illness .

On examination, the patient was conscious, oriented, and hemodynamically stable, without cyanosis, jaundice, Chest and cardiovascular examinations were unremarkable. Abdominal examination was also unremarkable. However, there was visible dilation of superficial veins in the left upper limb and left chest with associated swelling on the left side of the chest as shown above Fig1 . These veins were compressible, with no skin discolouration, no sensory or motor deficits compared to the right arm. Brachial, radial, and ulnar pulses were intact. The patient reported heaviness and pain when raising his arm above his head.
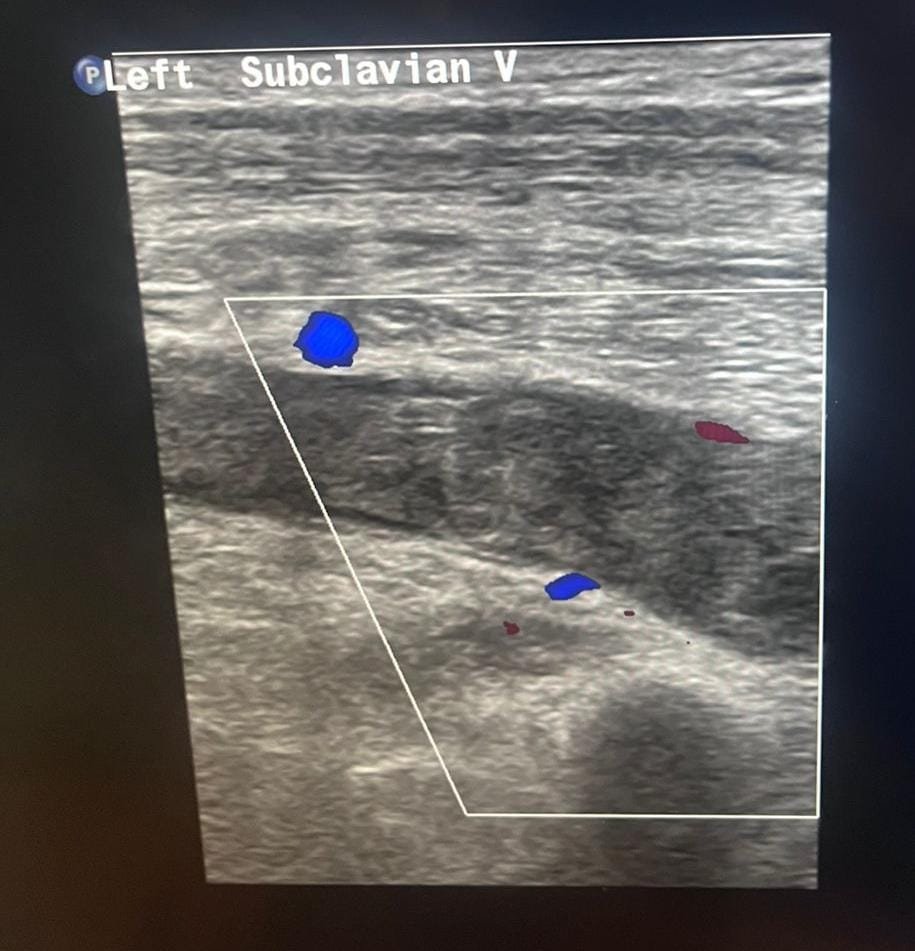
HE had normal investigations apart from doppler as shown below .Thrombotic screen was negative
Given the presentation, a diagnosis of Paget-Schroetter syndrome (PSS) was made. PSS is an effort-induced thrombosis of the axillary and subclavian veins, often associated with thoracic outlet compression. The patient was promptly started on anticoagulation therapy as part of the standard treatment approach and improved .He was discharged home with an advice to follow up
Paget-Schroetter Syndrome (PSS): Overview, History, and Treatment
Overview:
Paget-Schroetter syndrome (PSS), also known as effort-induced thrombosis, is a rare form of upper extremity deep vein thrombosis (UEDVT) that affects the axillary and subclavian veins. It is typically associated with repetitive upper limb movements, especially in young, active individuals or athletes engaging in activities such as weightlifting, baseball, or swimming. The condition arises due to compression of the subclavian vein at the thoracic outlet, leading to vascular injury, inflammation, and subsequent thrombosis.
Historical Background:
Paget-Schroetter syndrome was first described in 1875 by Sir James Paget, a British surgeon, who noted spontaneous thrombosis in the subclavian vein. Later, in 1884, Leopold von Schrötter, an Austrian physician, further elaborated on the vascular pathology associated with this condition, leading to its eponymous name.
Pathophysiology:
PSS occurs due to chronic mechanical compression of the subclavian vein as it passes through the thoracic outlet, a narrow passage between the collarbone and the first rib. Over time, repetitive microtrauma leads to endothelial damage, inflammation, and clot formation, resulting in obstruction of venous return. Patients typically present with:
- Swelling and discoloration of the affected limb
- Prominent, dilated superficial veins on the shoulder and chest (Urschel’s sign)
- Heaviness, pain, or tightness in the arm, especially with movement
- Cyanosis or dusky discoloration of the skin in some cases
Diagnosis:
The diagnosis is typically confirmed using imaging studies, including:
- Doppler ultrasound – Initial screening tool to detect venous thrombosis
- CT or MR venography – To assess the extent of thrombosis and any underlying venous compression
- Catheter-based venography – The gold standard for evaluating venous obstruction
Treatment:
Management of Paget-Schroetter syndrome involves a combination of medical and interventional therapies to restore venous patency and prevent complications. The main treatment strategies include:
- Anticoagulation Therapy – First-line treatment to prevent clot propagation and reduce the risk of pulmonary embolism. Commonly used agents include low-molecular-weight heparin (LMWH) and direct oral anticoagulants (DOACs).
- Thrombolysis – In cases of extensive clot burden, catheter-directed thrombolysis with agents like alteplase (tPA) is used to dissolve the clot.
- Surgical Decompression (Thoracic Outlet Decompression) – If venous compression is persistent or recurrent, surgical intervention (such as first rib resection or scalenectomy) may be required to relieve pressure on the subclavian vein.
- Balloon Venoplasty and Stenting – In some cases, endovascular techniques like balloon dilation or stenting may be considered to restore venous flow.
- Physical Therapy and Postural Correction – Patients are advised to modify activities, adopt postural changes, and undergo rehabilitation to prevent recurrence.
Prognosis:
With early diagnosis and appropriate treatment, the prognosis for PSS is generally favorable. However, delayed management can lead to complications such as chronic venous insufficiency, post-thrombotic syndrome, or pulmonary embolism.
Join the mailing list!
Get the latest articles delivered right to your inbox!



