
Psychiatric manifestation of an organic disease
Clinical case records :
Clinical scenario : A 35 year old female presented with history of increased talkativeness, quarrelsome attitude, forgetfulness, poor recognition of close relations, social withdrawal, aimless wandering of 3 weeks duration. With these symptoms she was brought to a local psychiatrist. She was started on anti psychotic medication but her symptoms continued . After 2 months she developed weakness of her right side of her body and was brought to medical emergency .
On examination :The patient was drowsy but arousable, however she was not oriented to time, place or person. She had no jaundice or lymphadenopathy. Her systemic examination was normal. The neurological examination revealed positive neck stiffness, right facial palsy and right hemiplegia. Her right side plantar was up going. Fundoscopic exam revealed papilloedema.
On evaluation :She was found to have leukocytosis (11200) with high erythrocyte sedimentation rate (60 min first hour). Her liver and renal function tests, serum calcium and phosphorous
were normal. ECG and x-ray chest revealed no abnormality. HIV serology was negative.
CT scan of the head revealed white matter edema of the left parieto-occipital region with mass effect on the left ventricle with midline shift suggestive of venous thrombosis. Contrast CT of the
head showed enhancement of these lesions suggestive of demyelination
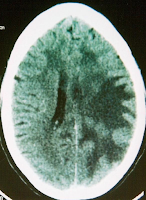 |
| Fig 1 Contrast enhanced CT scan showing mass effect and enhancement in Parietal lobes |
Management :
She was given decongestive therapy with intravenous Mannitol and lumbar puncture was done very carefully. Cerebrospinal fluid (CSF) analysis revealed a total leucocyte count of 210 cells with 85% lymphocytes, 15% neutrophils, CSF proteins 542 mg/dl, sugar 28 mg/dl, adenosine deaminase (ADA) levels were 27 IU (normal <10), TB polymerase chain reaction (PCR) was positive. On the basis of these findings a 4-drug regimen of antitubercular treatment (ATT) (Tab. INH 300 mg, Cap. Rifampcin 600 mg, Tab. Ethambutol 800 mg, Tab. Pyrazinamide 1.5 g and Tab. Pyridoxine 60 mg) was started. She was given Inj.Methylprednisolone 1 g I/V once daily for 5 days followed by oral steroids (Tab. Prednisolone 40 mg daily). Oral steroids were tapered over the next four weeks and ATT was continued. TB culture was positive after 6 weeks
The patient had progressive improvement in 8 weeks time and was discharged home . On discharge she was conscious, oriented to time place and person and had power of grade V in all four limbs. Repeat CT done after 4 weeks showed marked regression of edema
Message : Never miss an organic disease with psychiatric manifestation .
Join the mailing list!
Get the latest articles delivered right to your inbox!







